Cure and prevent diabetes mellitus with diet, not drugs
Part 3: Conventional Treatment mens a progression to ill health
Introduction
Conventionally, as diabetics are more at risk of heart disease and other
cardiovascular
complications, they are advised to eat 'healthily' and treated with a diet
based on
carbohydrates — bread, pasta, cereals and "five portions of fruit and
vegetables a day". They
are also told to cut down their fat intake.
Conventional wisdom also says that 80% of Type-2 Diabetes is associated with
obesity
which
in turn is said to be directly related to the increasing weight and decreasing
physical activity of
the population. It is believed by DiabetesUK that their low-fat,
carbohydrate-based diet will
help diabetics lose weight as this has enormous benefits.
So let us look at what a newly diagnosed diabetic patient can expect from
following the advice
of DiabetesUK and the American Diabetic Association.
Conventional Risk Factors for Type-2 are:
- Increasing age
- Physical inactivity
- Greater obesity
- Longer duration of obesity
- Unfavourable body fat distribution
- hyperinsulinaemia
There is little we can do about the first 'risk factor' as the alternative to getting older is dying young. Most of the rest are concerned with overweight.
Aim of Diabetes Treatment
It is the complications brought on by diabetes that are the real problem. Most
of these involve
the cardiovascular system through the glycosylation of haemoglobin (the coating
of
haemoglobin in the blood with sugar). Diabetics know this as HbA1c — it
is not a desirable
condition and the lower its measurement the better.
As most diabetic complications concern the cardiovascular system, the aim is to:
- Control hyperlipidaemia
- Control hyperglycaemia
- Control 'risk factors' to prevent diabetes
Lose weight — lose diabetes
If you are overweight, and most diabetics are, weight loss is normally the first concern for, if maintained, the potential benefits of weight loss are remarkable. (1) A weight loss of 10 kg:
- Reduces HbA1c more than Metformin (the most commonly used anti-glycaemic drug)
- Reduces diabetes-related deaths
- Improves blood lipids, without drugs
- Improves blood pressure, without drugs
Conventional Method
In the last century, diabetics were treated with a high-fat, low- or
no-carbohydrate diet. But
that regime was revised when 'healthy eating' was introduced by the COMA report
of 1984.
Diabetics are more likely to suffer from ischaemic heart disease than people
without diabetes.
Under these circumstances, it seemed unwise to continue the high-fat
recommendations. And
so DiabetesUK recommends a 'healthy' diet based largely on carbohydrates and
low in fat.
Conventional Advice — American Diabetic Association
For most people with diabetes, diet control is the key to managing this complicated disease. It is also extremely difficult. The current state of the diabetic diet is in flux, and at this time, there is no single diet that meets all the needs of everyone with diabetes. There are some constants, however. All people with diabetes should aim for healthy lipid (cholesterol and triglyceride) levels and control of blood pressure. People with type 1 diabetes and type 2 diabetics on insulin or oral medication must focus on controlling blood glucose levels by coordinating calorie intake with medication or insulin administration, exercise, and other variables. Adequate calories must be maintained for normal growth in children, for increased needs during pregnancy, and after illness. For overweight type 2 diabetics who are not taking medication, both weight loss and blood sugar control are important. A reasonable weight is usually defined as what is achievable and sustainable, rather than one that is culturally defined as desirable or ideal. And the general rules for healthy eating apply to everyone: limit fats (particularly saturated fats and trans-fatty acids), protein, and cholesterol, and consume plenty of fiber and fresh vegetables. Patients should meet with a professional dietitian to plan an individualized diet that takes into consideration all health needs.
Conventional Advice — DiabetesUK:
In a similar way, DiabetesUK say:
- "The healthy diet for people with diabetes is the healthy diet recommended for everyone."
- "Foods can be divided into five main groups. In order for us to enjoy a balanced diet we need to eat foods from these groups."
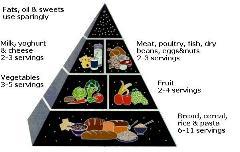
And like the American Diabetic association they lay things out in groups
— this time on a plate (left)
But note that in both these two pictures the foods recommended to form the
basis of all meals are predominantly carbohydrates — starches and sugars
in the form or bread, pasta, breakfast cereals, rice, fruit and vegetables.
These between them fill two-thirds of the plate. At the bottom, in the smallest
section we have fats and sugars — although fruit is mainly sugar and,
thus should, presumably be there as well. As we will see in
Part 4,
I believe that this is really nonsensical.
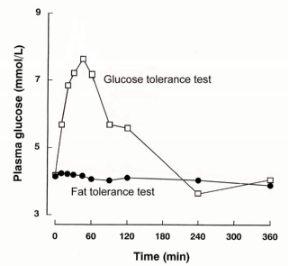
Glucose tolerance test To test for diabetes, patients are often given a glucose tolerance test. In this test, they drink a quantity of glucose and then their blood glucose is checked to see:
- How high it rises and
- How long it takes for their blood glucose to return to a normal level.
At the right you can see a typical glucose tolerance test for a healthy person.
Note that a similar tolerance test using fat does
not
raise blood glucose
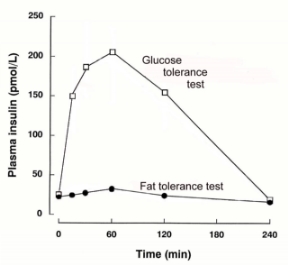
The effect on insulin
If we look at the effects of the two tolerance tests on blood insulin, we see a
similar pattern. Because high levels of glucose in the blood are harmful, this
rapid release into the bloodstream causes the pancreas to dump a large amount
of insulin into the bloodstream to bring that level down. As you can see,
insulin is produced very quickly — but it stays high much longer than
necessary. This means that when the blood glucose is down to a normal level,
after about 80 minutes, insulin is still near its highest point.
The consequence of this is that blood glucose is driven abnormally low, you
become hypoglycaemic, soon feel hungry, and so need to snack. In this way, you
eat more than your body needs, while the excess is stored out of the way as fat.
And, just as fat doesn't raise blood glucose, it also doesn't raise insulin.
This is why fats are so much healthier than carbs for a diabetic.
Are carb meals yo-yo tolerance tests?
But 100g of glucose is not dissimilar to the amount of carbohydrate —
starches and sugars — that would be consumed in a 'healthy' meal. And
their effect on blood glucose levels would be similar to that of the glucose
tolerance test.
This means that every time you have a 'healthy' meal of pasta, and fruit, with
mid-morning and mid-afternoon snacks of biscuits and/or sweets, your blood
glucose level will be continually rising and then brought down again by your
body's insulin — a form of yo-yo dieting by the hour, with your pancreas
working overtime.
What actually happens is that Carbohydrate Meals:
- Raise blood glucose levels.
- This in turn elevates levels of insulin on the blood
- That insulin takes excess energy (glucose) out of bloodstream.
- And that energy stored as fat.
- THE RESULT is: weight gain!
- But insulin also inhibits use of energy from fat cells.
- THE RESULT IS: no weight loss!
But, of course, weight loss is one of the major aims of the exercise.
And it gets worse:
Consequences of High Insulin Demand
As the pancreas is continulally being called uponn to produce large amounts of insulin, the following sequence of events takes place:
- Body demands for more insulin to reduce excessive blood glucose increase,
- Beta cells in the pancreas up-regulate or increase in size or capacity to meet that demand.
- Continual carb meals and insulin production leads to hypersensitivity.
- This leads to an exaggerated insulin response to even small carbohydrate loads. The flatter curve in the graph on the left demopnstrates that for the same stimulus far more insulin is produced.
- Hyperinsulinaemia (high levels of insulin in the bloodstream) leads to insulin resistance in fat and muscle cells.
- This increases glucose intolerance and insulin resistance.
- The pancreas has to produce even more insulin to be effective
- Until eventually, the pancreas is no longer able to cope and it gives up.
A senior NHS diabetic dietician, who must remain anonymous for obvious reasons, admitted that she had NEVER seen ANYONE with type 2 diabetes able to control blood sugar on the standard high carb diet!
So Bring on the Drugs!
As dietary control fails, drugs are employed to reduce glucose levels.
There are basically four classes of drug used to reduce levels of glucose in
the blood:
1. Alpha-glucosidase inhibitors — retard glucose uptake from the
intestines (Acarbose)
2. Biguanides — augment muscular uptake of glucose (Metformin)
3. Sulphonylureas — stimulate insulin production by pancreas (Glimepiride)
4. Prandial glucose regulators — stimulate insulin release from pancreas
The first class of drugs slow down the rate at which glucose enters the
bloodstream and the
second takes it out of the bloodstream for storage in the muscles as glycogen.
But the body
can only store so much glycogen. So other drugs (3 and 4) are used to increase
the amount of
insulin in the blood. This increases the removal of glucose but, as it does so
by storing the
excess glucose as fat, this results in weight gain — the exact opposite
of what doctors are
trying to achieve.
Polypharmacy May Be Unavoidable
And weight gain is not the only problem. Because of the increased risk that
diabetics have of
complications, polypharmacy, (the use of many drugs together) is a real
concern. A paper
published in the
British Medical Journal
pointed out that:
(2)
Given the cardiovascular risk profile of type 2 diabetes, up to 10% of patients
could require:
- Two or three hypoglycaemic agents (ultimately including insulin),
- At least three antihypertensive agents,
- Two hypolipidaemic agents,
- And aspirin.
- "A high proportion will also require treatment for coexistent cardiovascular disease and coincidental unrelated chronic disease."
"It is difficult to see how we can realistically expect patients to comply for long with such a draconian regimen requiring so many separate drugs."
ID-NIDDM?
Polypharmacy is only part of the deterioration in quality of life a diabetic on
conventional
treatment can expect.
As conventional low-fat diets and drugs fail and glycaemic control
deteriorates, eventually
insulin is prescribed. Over time, therefore, some non-insulin dependent
diabetics end up
requiring insulin injections. So they are now insulin dependent, non-insulin
dependent,
diabetics! This elevates insulin levels in the blood even further — it's a
condition called
hyperinsulinaemia. And it is not a healthy progression as it increases the risk
of even more
serious disease.
And remember that hyperinsulinaemia is also a risk factor for diabetes!!
The complications of Insulin
Firstly, insulin puts on weight. Its purpose is to take energy out of the bloodstream and store it as fat — the very thing that conventional treatment is aimed at stopping. For this reason:
- Insulin is the most fattening hormone.
- Diabetics who have to inject insulin find it almost impossible to lose weight.
But weight gain is not the only complication of insulin use, as insulin:
- Increases risk of thrombosis
- Increases plaque formation
- Prevents plaque regression
- Stimulates connective tissue synthesis
- Stimulates IGF-1 (3)
Insulin elevates blood pressure by:
- Kidney Na+ retention
- Enhancing flow of Na+ and Ca++ to vascular smooth muscle cell
- Fasting and postprandial insulin levels have significant positive associations with systolic and diastolic BP (4)
Hyperinsulinaemia (high blood insulin level) is also known to be involved in:
- Polycystic ovarian syndrome (PCOS)
- Prostate cancer,
- Endometrial cancer,
- breast cancer.
And it is suspected in relation to:
- Gestational hypertension
- Preeclampsia
- and Osteoporosis (5)
Insulin increases heart disease risk
The most important complication of diabetes is the large increase in risk of a
heart
attack.
A recent study of subjects in Framingham, Massachusetts demonstrated that a
blood clot is
much more likely to occur if insulin levels are increased. This effect was
present in individuals
who did not have diabetes, but was more profound in individuals who did have
diabetes.
(6)
Blood clots (thromboses) are a recognised cause of heart attacks, strokes,
blockages in other
arteries and deep vein thrombosis.
Insulin increases cancer risk
Breast cancer patients with high levels of insulin in their blood seem to be
more likely to die of
their disease. Researchers found that insulin may predict whether a woman's
breast cancer
recurs after therapy and whether she will die.
In a study of 535 breast cancer patients followed for up to 10 years, those
with the highest
insulin levels were more than eight times more likely to die and were almost
four times as
likely to have their cancer recur at a distant site.
(7)
Although many of the women in the study were obese, and obesity is known to
affect both
breast cancer prognosis and insulin levels, obesity alone did not completely
explain the link
between insulin and poorer cancer survival. Insulin normally helps promote cell
growth.
Researchers hypothesize that in the breast, insulin can spur the growth of both
normal and
cancerous cells.
The insulin/cancer risk found confirmation in another study conducted at the
Samuel
Lunenfeld Research Institute, Mount Sinai Hospital. This study demonstrated
that patients
with the highest levels of insulin in their blood were twice as likely to have
their cancer spread
and more than three times as likely to die of the cancer compared to patients
with low levels of
insulin in their blood.
(8)
Recap on Conventional Approach
Major aims are:
- Weight loss.
- Control of cardiac risk factors.
BUT:
- The conventional high-carb, low-fat diet results in hyperglycaemia.
- Hyperglycaemia causes hyperinsulinaemia.
- Excess energy is stored as body fat.
- Weight gain is the norm and cardiac risks are increased.
Thus conventional treatment for diabetes, using a diet based on breads, pasta and fruit is likely to do the exact opposite of what is aimed for — and make the condition worse. Why that happens is explained in detail in Part 4: Why carbs are the wrong foods for diabetics
References
1.
Jung RT. Obesity as a disease.
Br Med Bull
1997; 53: 307-21.
2.
Winocour PH. Effective diabetes care: a need for realistic targets.
BMJ
2002;324:1577-1580
3.
DeFronzo RA, Eleuterio F. Insulin resistance: a multifaceted syndrome
responsible for
NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular
disease.
Diabetes Care
1991; 14: 173-91. and Meigs JB, Mieeleman MA, Nathan DM, et al.
Hyperinsulinemia, hyperglyceima, and impaired hemostasis. The Framingham
offspring study.
JAMA
2000;283:221-229.
4.
DeFronzo RA, Eleuterio F. Insulin resistance: a multifaceted syndrome
responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic
cardiovascular disease.
Diabetes Care
1991; 14: 173-91.
5.
Bachman JM The low-carbohydrate diet in primary care ob/gyn.
Prim Care Update
Ob/Gyn.
2001; 8: 12-17
6.
Meigs JB, Mieeleman MA, Nathan DM, et al. Hyperinsulinemia, hyperglyceima, and
impaired hemostasis. The Framingham offspring study.
JAMA
2000; 283: 221-229.
7.
Annual meeting of American Society of Clinical Oncology, New Orleans, 23 May
2000
8.
Goodwin PJ, Ennis M, Pritchard KI, Trudeau ME, et al. Fasting insulin and
outcome in
early-stage breast cancer: results of a prospective cohort study.
J Clin Oncol
2002; 20: 42-51
Introduction
Part 1: The scale of the problem
Part 2: What is diabetes -- Are you at risk?
Part 3: Conventional treatment for Type-2 diabetes — and why it fails
Part 4: Why carbs are the wrong foods for diabetics
Part 5: The evidence
Part 6: The correct diet for a Type-2 diabetic, (or treatment without drugs)
Part 7: Treatment for Type-1 diabetes
Suitable foods for diabetics
Last updated 6 February 2008

 HOME
HOME